How To Pay And Indian Health Services Bill
Indian Health Service (IHS)
- Indian Health Service (IHS)
- IHS Provider
- Urban Indian Organization (UIO)
- Early and Periodic Screening, Diagnostic, and Handling (EPSDT)
- Billing Information
- Indian Health Service (IHS) Benefits
- Coding
- UB-04 Paper Claim Reference Table
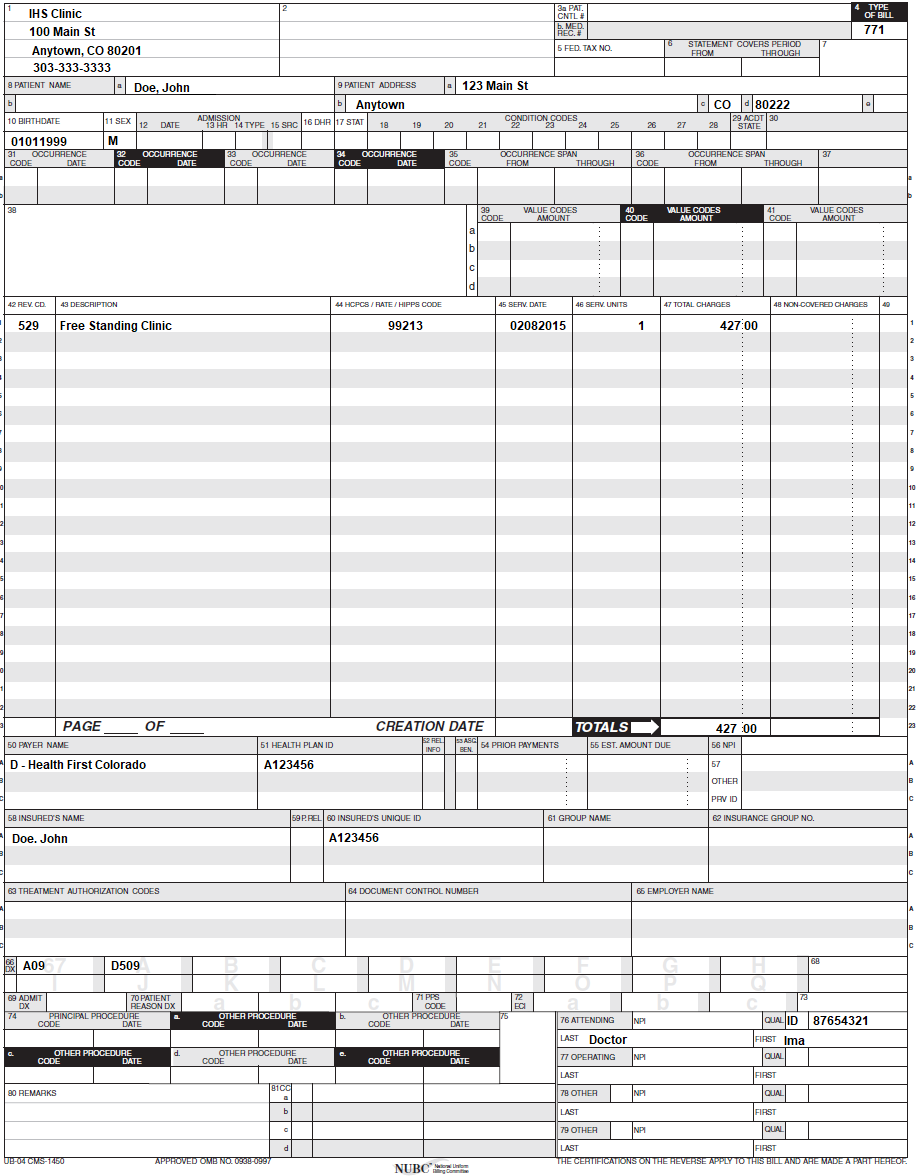
- UB-04 Outpatient Claim Example
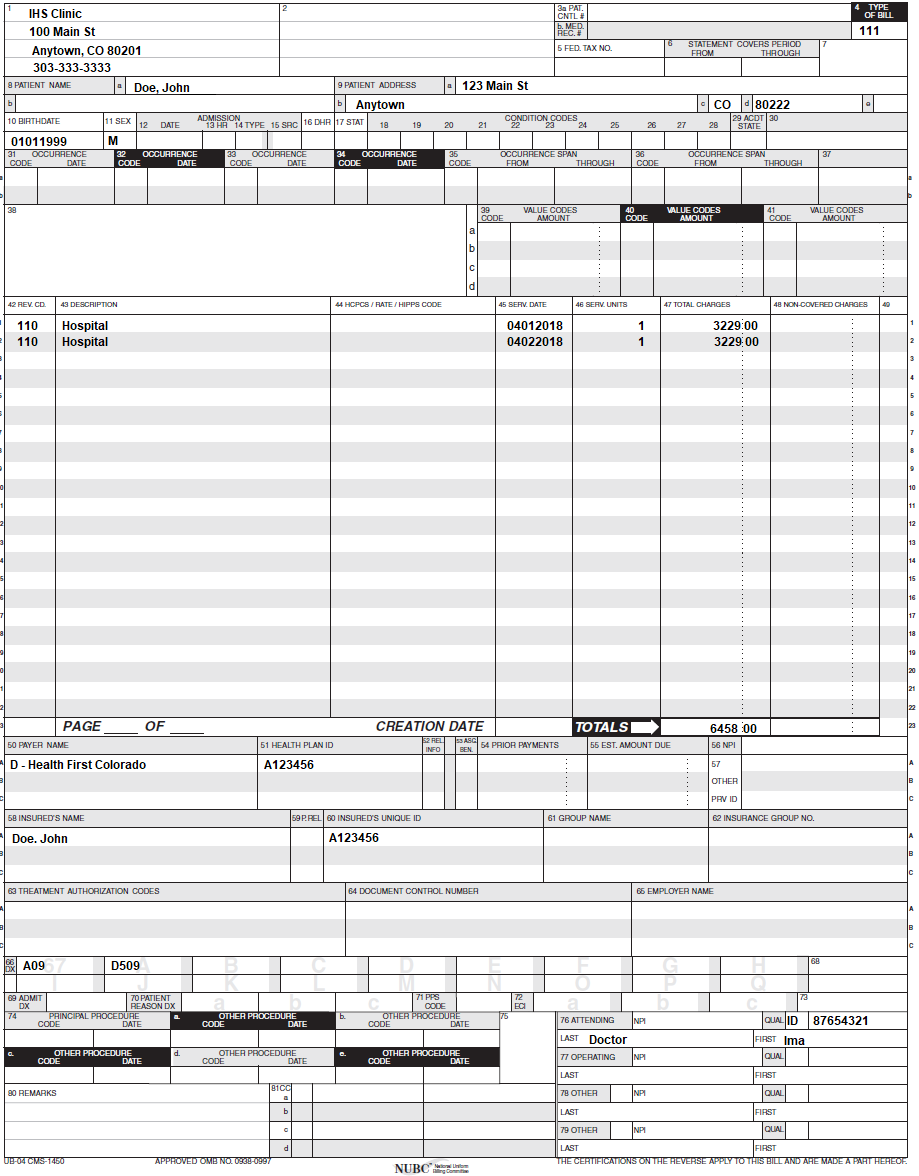
- UB-04 Inpatient Merits Instance
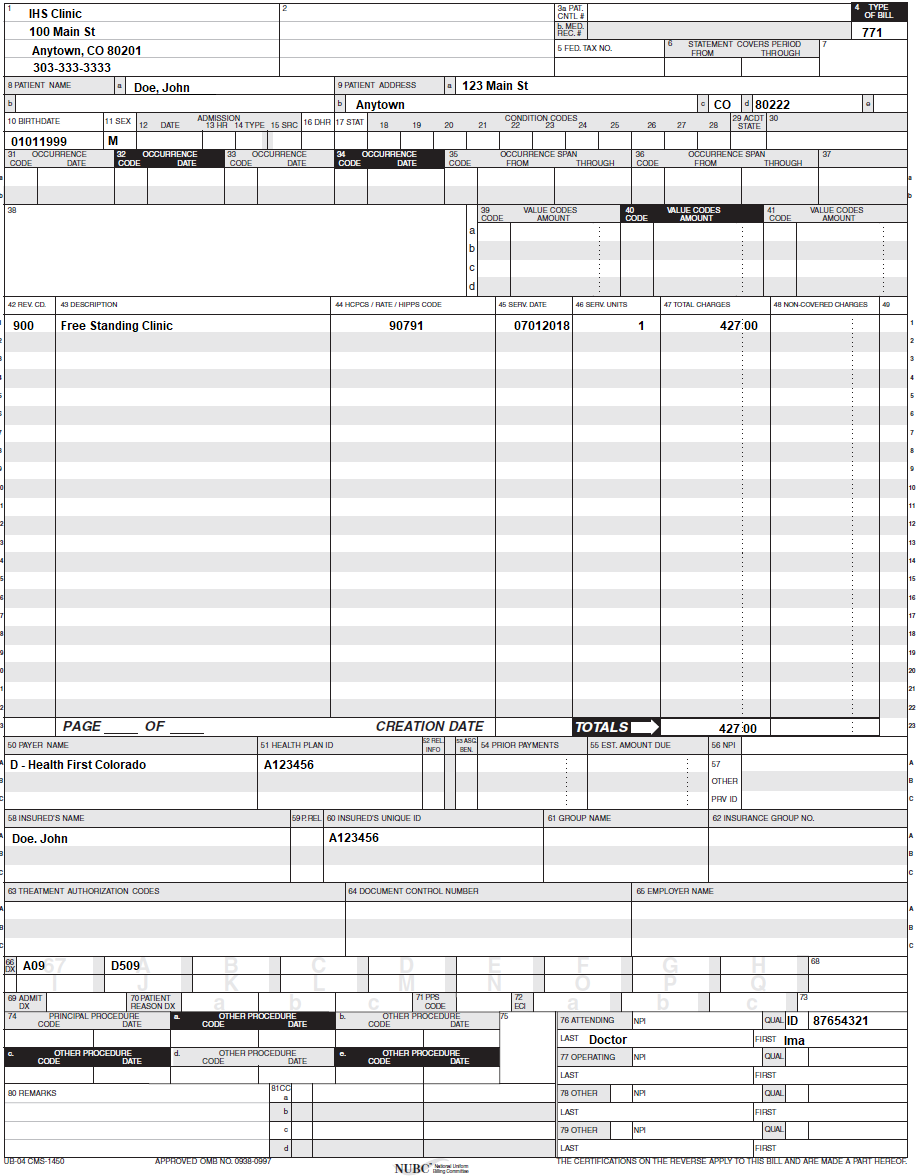
- UB-04 Behavioral Health Claim Instance
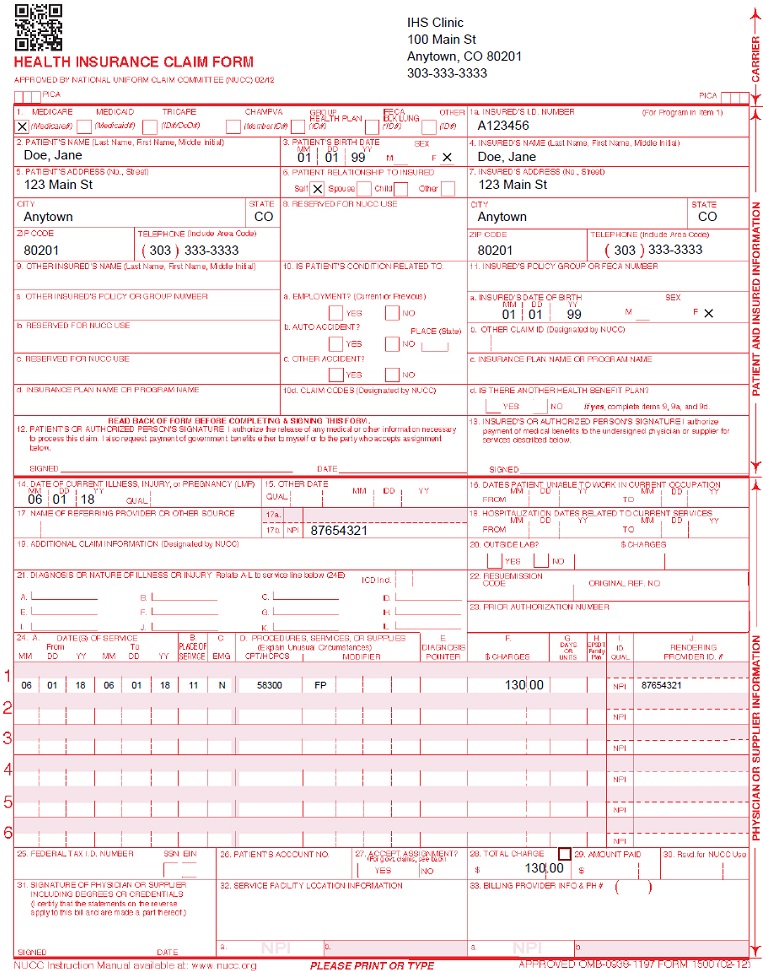
- CMS 1500 Professional Claim Example
- Sterilizations, Hysterectomies, and Abortions
- Timely Filing
- IHS Revisions Log
Return to Billing Manuals Web Page
Indian Wellness Service (IHS)
Providers must exist enrolled equally a Health Showtime Colorado (Colorado's Medicaid Program) provider in club to:
- Treat a Health Outset Colorado member
- Submit claims for payment to Health First Colorado
Providers should refer to the Code of Colorado Regulations, Program Rules (10 C.C.R. 2505-ten 8.700), for specific information when providing FQHC and RHC services.
NOTE: Wellness Offset Colorado should be billed only in the result that an eligible American Indian Alaska Native (AIAN) fellow member is enrolled in Wellness Starting time Colorado. If the eligible member also possesses a third-party insurance plan, the individual plan must exist billed first. Any services not covered by the private insurance programme that are covered by Health First Colorado may then be billed. In the event an eligible AIAN fellow member is dually eligible for Medicare and Health Start Colorado, Medicare must be billed get-go. Whatsoever services not covered by Medicare that are covered by Health First Colorado may then exist billed.
Back to Top
IHS Provider
In guild to bill as an IHS provider with Health Starting time Colorado, the treatment facility must reside on land owned and operated by a federally recognized tribe as defined under Title 4 of the Indian Health Care Improvement Act.
Back to Top
Urban Indian Organization (UIO)
Urban Indian Organizations (UIO) are currently ineligible to receive IHS designation under federal law. Even so, UIOs may apply to become a federally qualified wellness center (FQHC) with Health First Colorado, as long as they receive funds under Title V of the Indian Health Care Improvement Deed.
Back to Top
Early on and Periodic Screening, Diagnostic, and Treatment (EPSDT)
8.280.iv.E Other EPSDT Benefits
Other wellness care services may include other EPSDT benefits if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All goods and services described in Department 1905(a) of the Social Security Human activity are a covered benefit under EPSDT when medically necessary every bit defined at 10 C.C.R. 2505-10, Department viii.076.1.eight, regardless of whether such goods and services are covered nether the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a proficient or service that volition, or is reasonably expected to, help the client to attain or maintain maximum functional capacity in performing one or more Activities of Daily Living; and meets the criteria set forth at Department 8.076.1.8.b - g.
- The service provides a condom environment or situation for the child.
- The service is not for the convenience of the caregiver.
- The service is medically necessary.
- The service is not experimental or investigational and is generally accepted by the medical customs for the purpose stated.
- The service is the least plush.
Billing Information
Refer to the General Provider Information manual for general billing data.
Back to Summit
Indian Wellness Service (IHS) Benefits
Outpatient Services
Payment for outpatient services rendered shall be paid per visit/encounter. Rates are determined by the U.South. Department of Wellness and Human being Services and are published each year in the Federal Register. Wellness Offset Colorado covers the followingoutpatient services:
- Medical services
- Behavioral wellness services
- Hospital outpatient services
- Podiatry services
- Optometry services
- Radiology services
- Laboratory services
Health Offset Colorado shall reimburse multiple visit/encounter claims for a member on the same date of service by the same facility based on the following conditions:
- If the services provided are for different diagnoses and the claims each accept a unlike diagnosis ICD-10 code, or
- If the services are in the categories of either medical, clinical laboratory, or radiology, based on the process lawmaking detail of the merits. If all iii types of services are rendered then these iii split up claims may be billed:
- Clinical Laboratory procedure codes.
- Radiology procedure codes.
- Medical services would be any other medical procedure code not in the Clinical Laboratory or Radiology category.
Behavioral wellness servicesare a covered benefit. Behavioral health services must be billed using Revenue Lawmaking 900. Claims must be billed direct to Health Starting time Colorado. These services are reimbursed the IHS outpatient encounter charge per unit.
Inpatient Services
Health First Colorado coversinpatient servicesat IHS facilities. Payment for services rendered shall exist per date of inpatient stay and is set in the Federal Register past the U.Southward. Department of Health and Human Services. Health Kickoff Colorado shall brandonly one payment per date of service per member.
Professional Services
Professional servicesrendered by IHS providers at an inpatient hospital or ambulatory surgical middle are billed on the professional person claim type (837p/CMS1500) and are reimbursed at the Fee Schedule charge per unit. Providers should refer to the billing manual for medical and surgical services found on the Billing Manuals web page under the CMSS 1500 driblet-downwards menu. Covered services include anesthesia services, obstetric services, medical services, vaccine/immunization services, psychiatric services, and surgical services equally detailed in the medical and surgical services billing transmission (run across link above).
Pharmacy services rendered by an IHS pharmacy are covered past Health Starting time Colorado, instructions can be found in the pharmacy billing manual.
Dental servicesare covered by Health First Colorado, only must be billed to DentaQuest. For more than information, see locator 42 on folio xi of this manual.
Urban Indian Organizations (UIO)who are designated as federally qualified health centers (FQHC) with Health Get-go Colorado who use cost reports in lieu of the federal encounter rate should refer to the billing transmission for FQHCs institute on the Billing Manuals web page under the UB-04 drop-down menu.
Dorsum to Meridian
Coding
IHS facilities are required to employ revenue codes to neb Health First Colorado. The valid revenue codes for reimbursement are:
| Revenue Lawmaking | Type of Service |
|---|---|
| 529 | Concrete Health (Outpatient) |
| 900 | Behavioral Health (Outpatient) |
| 110 | Inpatient Services (Physical and Behavioral Wellness) |
IHS services are priced at an encounter rate. All routine services are included in the come across rate. Encounter rates for Tribal-FQHCs and IHS facilities are adamant by the federal Department of Wellness and Human being Services and are published in the Federal Annals for each calendar year.
In order to provide the Health Offset Colorado programme with basic clinical information for utilise in evaluating services requested and received past Health Outset Colorado members, IHS and Tribal-FQHCs are required to include all procedure codes (CPT and HCPCS codes) for services provided during a visit on claims. To be reimbursed, a Tribal-FQHC or IHS facility that submits a UB-04 or 837 Institutional (837I) electronic transaction must have at to the lowest degree ane (1) claim line that identifies revenue lawmaking 0529. All other lines on the merits should have the revenue lawmaking most appropriate for the service. The line item with revenue code 0529 or 0521 can appear at any line on the claim and with whatsoever procedure lawmaking.
Back to Summit
UB-04 Newspaper Claim Reference Table
The data in the following table provides instructions for completing form locators (FL) as they appear on the paper UB-04 claim form. Instructions for completing the UB-04 claim form are based on the electric current National Uniform Billing Committee (NUBC) UB-04 Reference Manual. Unless otherwise noted, all data form locators on the UB-04 have the same attributes (specifications) for Wellness First Colorado as those indicated in the NUBCUB-04 Reference Manual.
All code values listed in the NUBC UB-04 Reference Transmission for each form locatormay notexist used for submitting paper claims to Health Get-go Colorado. The advisable lawmaking values listed in this manual must exist used when billing Health First Colorado.
The UB-04 Certification document (located subsequently the Sterilizations, Hysterectomies, and Abortions instructions and in the Provider Services Forms section) must be completed and attached to all claims submitted on the paper UB-04. Completed UB-04 newspaper Health Commencement Colorado claims, including hardcopy Medicare claims, should be mailed to the correct fiscal agent address listed in Appendix A, under the Appendices drop-downwards section on the Billing Manuals web page.
The Paper Merits Reference Table below lists the required, optional, or provisional form locators for submitting the newspaper UB-04 claim form to Wellness Outset Colorado for FQHC and RHC services.
| Form Locator and Labels | Completion Format | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Billing Provider Name, Address, Phone Number | Text | Abbreviate the state using standard postal service office abbreviations. Enter the telephone number.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Pay-to Name, Accost, Metropolis, State | Text | Required simply if different from FL 1. Enter the provider or agency name and complete mailing address of the provider who will receive payment for the services:
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3a. Patient Control Number | Upward to 20 characters: Letters, numbers or hyphens | Optional Enter data that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Communication (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3b. Medical Record Number | 17 digits | Optional Enter the number assigned to the member to assist in retrieval of medical records. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Type of Bill | 3 digits | Required IHS: Apply type of Bill 71X or 77X for outpatient, 111 for inpatient.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| five. Federal Tax Number | None | Submitted information is not entered into the claim processing arrangement. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| half dozen. Statement covers period From/Through | From:6 digits MMDDYY Through: 6 digits MMDDYY | Required Each date of service must be billed on a dissever line. Split an entire calendar month into ii claims. This FL must reverberate the showtime and ending dates of service listed on the detail dates of service lines. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8a. Patient Identifier | Submitted information is non entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8b. Patient Name | Up to 25 characters, letters & spaces | Required Enter the member's last name, first proper name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Patient Accost - Street | Characters Letters & numbers | Required Enter the member's street/post office box as determined at the time of access. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Patient Address - City | Text | Required Enter the fellow member'south city as determined at the time of admission | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Patient Accost - State | Text | Required Enter the fellow member'due south state as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Patient Address - ZIP | Digits | Required Enter the fellow member's nada lawmaking equally determined at the fourth dimension of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9e. Patient Address - Country Lawmaking | Digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| x. Birthdate | 8 digits (MMDDYYYY) | Required Enter the member'south birthdate using two digits for the calendar month, 2 digits for the date, and four digits for the year (MMDDYYYY format). Example: 01012010 for January 1, 2010. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Patient Sex | 1 letter of the alphabet | Required Enter an M (male) or F (female) to point the member's sex. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Access Appointment | 6 digits | Non Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Admission Hour | 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Admission Type | ane digit | Provisional Consummate for emergency visits. one - Emergency Fellow member requires immediate intervention every bit a result of astringent, life-threatening or potentially disabling atmospheric condition. Exempts outpatient hospital claims from co-payment and PCP referral but if Acquirement Lawmaking 0450 or 0459 is nowadays. This is the merely do good service for an undocumented alien. If bridge billing, emergency services cannot be included in the span bill and must be billed separately from other outpatient services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| fifteen. Source of Access | ane digit | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| sixteen. Belch Hour | 2 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Patient Discharge Status | 2 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18-28. Weather condition Codes | ii digits | Conditional Complete with every bit many codes necessary to identify conditions related to this pecker that may touch payer processing.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Accident Country | 2 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31 - 34. Occurrence Code/Date | 2 digits & six digits | Conditional Complete both the code and date of occurrence. Enter the appropriate code and the date on which it occurred. Enter the date using MMDDYY format. Occurrence Codes:
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 35-36. Occurrence Span Code From/ Through | ii & half-dozen digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 38. Responsible Party Name/Address | None | Leave blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 39 - 41. Value Codes and Amounts | 2 characters and up to ix digits | Provisional Enter advisable codes and related dollar amounts to identify monetary data or number of days using whole numbers, necessary for the processing of this merits. Never enter negative amounts. Codes must be in ascending gild. If a value code is entered, a dollar amount or numeric value related to the code must ever exist entered.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 42. Revenue Code | 3 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 43. Revenue code Description | Text | Required Enter the revenue code description or abbreviated description. When reporting an NDC:
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 44. HCPCS/Rates/ HIPPS Rate Codes | v digits | Required Medical Claims - There may be multiple lines, each identified by revenue code 529 in locator 42. For each line enter a valid CPT lawmaking or HCPCS code that reflects the services rendered during the run into. This includes any medical, laboratory, radiology, physical therapy, occupational therapy, pharmacy, supply or other service rendered during the see. When a line identifies revenue code in the range of 0631-0636, the HCPCS will be required and an NDC. CPT and HCPCS codes cannot be repeated for the same date of service. Combine the units in FL 46 (Units) to report multiple services. On dental claims the D-code must exist put in locator 44 on each line for dates of services prior to July 1, 2014. For dates of services afterwards July 1, 2014, refer to the Office Reference Manual (ORM) nether 'DentaQuest Resources' located on the Dentist page of DentaQuest's website. Behavioral Health Claims - There may be multiple lines, each identified by acquirement code 900 in locator 42. For each line enter a curt-term behavioral health service code that reflects the service rendered during the encounter. HCPCS codes cannot be repeated for the same appointment of service. Combine the units in FL 46 (Units) to report multiple services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 45. Service Date | 6 digits | Required Enter the date of service using MMDDYY format for each detail line completed. Each date of service must autumn within the engagement span entered in the "Statement Covers Period" (FL vi). Not required for single date of service claims. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 46. Service Units | Up to three digits | Required Enter a unit value on each line completed. Use whole numbers merely. Do not enter fractions or decimals and exercise not show a decimal bespeak followed by a 0 to designate whole numbers (e.grand., Practice not enter 1.0 to signify ane unit) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 47. Total Charges | Upward to nine digits | Required Enter the full accuse for each line particular. Calculate the full charge as the number of units multiplied past the unit accuse. Exercise not subtract Medicare or third-party payments from line charge entries. Do non enter negative amounts. A yard total in line 23 is required for all charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 48. Not-covered Charges | Up to ix digits | Required Enter incurred charges that are non payable by Wellness Starting time Colorado. Non-covered charges must be entered in both FL 47 (Full Charges) and FL 48 (Non-Covered Charges). Each cavalcade requires a chiliad total. Non-covered charges cannot exist billed for outpatient hospital laboratory or hospital-based transportation services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| l. Payer Name | ane letter and text | Enter the payment source code followed past name of each payer system from which the provider might expect payment. At least one line must indicate Health First Colorado.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 51. Health Plan ID | 8 digits | Required Enter the provider'southward Wellness Plan ID for each payer proper noun. Enter the viii-digit Health First Colorado Program provider number assigned to the billing provider. Payment is made to the enrolled provider or agency that is assigned this number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 52. Release of Data | None | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 53. Assignment of Benefits | None | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 54. Prior Payments | Upwardly to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter 3rd party and/or Medicare payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 55. Estimated Amount Due | Up to nine digits | Conditional Consummate when there are Medicare or third-political party payments. Enter the net amount due from Health Get-go Colorado after provider has received other third party, Medicare or fellow member liability amount. Medicare Crossovers Enter the sum of the Medicare coinsurance plus Medicare deductible less 3rd-political party payments and member payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 56. National Provider Identifier (NPI) | x digits | Required Enter the billing provider's 10-digit National Provider Identifier(NPI). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 57. Other Provider ID | Submitted data is not entered into the merits processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 58. Insured's Name | Up to 30 characters | Required Enter the fellow member'due south name on the Health First Colorado line. Other Insurance/Medicare Consummate boosted lines when there is third party coverage. Enter the policyholder'south final name, first proper noun, and eye initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| sixty. Insured'south Unique ID | Up to 20 characters | Required Enter the insured's unique identification number assigned past the payer arrangement exactly as it appears on the health insurance card. Include letter prefixes or suffixes shown on the carte. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 61. Insurance Group Name | fourteen letters | Conditional Complete when in that location is third party coverage. Enter the proper name of the group or programme providing the insurance to the insured exactly as it appears on the health insurance bill of fare. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 62. Insurance Group Number | 17 digits | Conditional Consummate when at that place is third political party coverage. Enter the identification number, control number, or lawmaking assigned by the carrier or fund administrator identifying the group under which the private is carried. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 63. Handling Authorization Code | Up to 18 characters | Conditional Complete when the service requires a PAR. Enter the authorization number in this FL if a PAR is required and has been approved for services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 64. Document Control Number | Provisional | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 65. Employer Proper noun | Text | Conditional Complete when there is third party coverage. Enter the proper noun of the employer that provides health intendance coverage for the private identified in FL 58 (Insured Name). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 66. Diagnosis Version Qualifier | Submitted information is not entered into the merits processing system. Enter applicative ICD indicator to identify which version of ICD codes is beingness reported. 0ICD-10-CM (DOS 10/1/15 and later on) 9ICD-ten-CM (DOS 9/30/xv and before) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67. Master Diagnosis Code | Up to 6 digits | Required Enter the exact diagnosis code describing the principal diagnosis that exists at the time of admission or develops subsequently and affects the length of stay. Do not add extra zeros to the diagnosis code. Utilize diagnosis lawmaking Z00.00-10 Z00.110-Z00.111 Z00.121-Z00.129 Z00.6-Z00.8 Z02.0-Z02.6 Z02.81-Z02.89 Z76.2 for EPSDT screenings. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67A. - 67Q. - Other Diagnosis | six digits | Optional Enter the exact diagnosis lawmaking respective to additional conditions that co-exist at the time of access or develop afterwards and which result the treatment received or the length of stay. Do non add extra zeros to the diagnosis code. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 69. Admitting Diagnosis Code | 6 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 70. Patient Reason Diagnosis | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 71. PPS Code | Submitted information is not entered into the merits processing arrangement. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 72. External Cause of Injury code (E-Lawmaking) | 6 digits | Required if known Enter the diagnosis code for the external cause of an injury, poisoning, or adverse effect. This lawmaking must begin with an "Eastward". | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74. Chief Procedure Code/Appointment | 7 characters and half dozen digits | Conditional Enter the procedure code for the principal process performed during this billing menstruum and the date on which procedure was performed. Enter the engagement using MMDDYY format. Apply the following criteria to determine the principle procedure:
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74A. Other Process Code/Date | seven characters and 6 digits | Conditional Complete when there are additional significant procedure codes. Enter the procedure codes identifying all meaning procedures other than the main procedure and the dates on which the procedures were performed. Report those that are most important for the episode of care and specifically any therapeutic procedures closely related to the principal diagnosis. Enter the engagement using MMDDYY format. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 76. Attending NPI - Required Attending Concluding/Offset Name | NPI - 10 digits Text | Health Beginning Colorado ID Required NPI - Enter the 10-digit NPI number assigned to the physician having primary responsibleness for the member'south medical care and treatment. This number is obtained from the md and cannot be a clinic or group number. (If the attending physician is not enrolled in Health First Colorado or if the member leaves the ER before existence seen by a physician, the hospital may enter their private numbers.) Hospitals and FQHCs may enter the member's regular md's 10- digit NPI in the Attending Physician ID form locator if the locum tenens dr. is not enrolled in Wellness Get-go Colorado. QUAL - Enter "1D" for Medicaid Enter the attending doctor's concluding and kickoff proper name. This course locator must exist completed for all services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 77. Operating NPI | Submitted information is not entered into the claim processing organization. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 78 - 79. Other ID NPI - Provisional | NPI - x digits | Conditional Consummate when attending physician is not the PCP or to identify additional physicians. NPI - Enter up to two 10-digit NPI numbers, when applicable. This form locator identifies physicians other than the attending physician. If the attention doctor is non the PCP or if a clinic is a PCP agent, enter the PCP NPI number equally the referring doctor. The name of the Wellness First Colorado member's PCP appears on the eligibility verification. Review either for eligibility and PCP. Health Get-go Colorado does non require that the PCP number appear more than once on each claim submitted. The attending md'southward last and first name are optional. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 80. Remarks | Text | Enter specific additional data necessary to process the merits or fulfill reporting requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 81. Lawmaking - QUAL/CODE/VALUE (a-d) | Qualifier: 2 digits Taxonomy Code: 10 digits | Optional Complete both the qualifier and the taxonomy code for the billing provider in field 81CC-a. Field 81CC-a must be billed with qualifier B3 for the taxonomy code to be captured in the claims processing system. If B3 is missing, no taxonomy lawmaking will be captured in the claims processing system. Only one taxonomy code can exist captured from field 81CC. If more than than one taxonomy lawmaking is provided, only the first instance of B3 and taxonomy code volition be captured in the claims processing arrangement. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Dorsum to Top
UB-04 Outpatient Merits Example
Back to Top
UB-04 Inpatient Claim Example
Dorsum to Top
UB-04 Behavioral Health Claim Example
Dorsum to Tiptop
CMS 1500 Professional person Claim Example
Back to Top
Sterilizations, Hysterectomies, and Abortions
For information on this topic, please see the Sterilization, Hysterectomies, and Abortions section in the Obstetrical and Reproductive Wellness Billing Manual located on the Department's billing manual web folio, nether CMS 1500 > Obstetrical Care.
Back to Top
Timely Filing
For more data on timely filing policy, including the resubmission rules for denied claims, delight see the General Provider Information manual located on the Department'southward billing manual web page.
Back to Top
IHS Revisions Log
| Revision Date | Changes | Made by |
|---|---|---|
| 08/07/2018 | Manual created | Section |
| 04/22/2019 | Updated inpatient acquirement code | Section |
| 06/19/2019 | Updated Appendices links and circumlocution | DXC |
| ten/02/2019 | Updated Procedure Code/HCPCS | Department |
| 12/02/2019 | Converted to web page | Department |
| 8/vii/2020 | Updated detail 81 of the Paper Claim Reference Tabular array for taxonomy code billing | DXC |
| x/7/2020 | Changes made to Process Code Requirements | Department |
| ii/1/2021 | Updated the billing and coding portion to include multiple come across policy for medical, lab, and radiology services. | Department |
| 7/seven/2021 | Updating with the standard EPSDT policy language | HCPF |
Back to Tiptop
Source: https://hcpf.colorado.gov/IHS-billing-manual
Posted by: dentonnevard.blogspot.com


0 Response to "How To Pay And Indian Health Services Bill"
Post a Comment